Translate this page into:
Camouflaged cardiac alert: Correlation of breast arterial calcification with carotid intima media thickness for evaluation of cardiac risk

*Corresponding author: Bhawna Dev, Department of Radiology, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai, India. bhawnadev@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ingole SU, Dev B, Varadarajan S, Balakrishnan SS, Goyal N, Chinnappan S, et al. Camouflaged cardiac alert: Correlation of breast arterial calcification with carotid intima media thickness for evaluation of cardiac risk. Indian J Breast Imaging 2023;1:25-30.
Abstract
Objectives:
To determine the association between breast arterial calcification (BAC) and carotid intima-media thickness (C-IMT) and, in turn, predict the risk of cardiovascular events. To independently access its relationship with other co-morbidities like diabetes mellitus (DM), hypertension (HTN), and menopause with BAC.
Material and Methods:
A total of 540 patients (270 with BAC and 270 without BAC) in the age group of 40–60 years who underwent mammograms at our institution between April 2021 to October 2021 were included in the study. In addition, an ultrasound was performed to evaluate the intima-media thickness in bilateral common carotid arteries 1 cm proximal to the carotid bulb. The mean C-IMT between the two groups (patients with and without BAC) was compared to understand the relationship between C-IMT and BAC. The independent relationship of BAC was also evaluated with the risk of co-morbidities like DM, HTN, and menopause.
Results:
The median C-IMT was higher in the group with BAC (0.85 mm, interquartile range (IQR) = 0.2) than in the group without BAC (0.6 mm, IQR = 0.10), which is statistically highly significant with p < 0.001. Further analysis among subgroups of age and DM also revealed IMT to be significantly higher in the group with BAC (0.85 mm, IQR = 0.20) compared to those without BAC (0.6 mm, IQR = 0.15) (p < 0.001). The median age in patients with BAC was significantly higher (57 years, IQR = 10 years) than those without BAC (48 years, IQR = 11.8 years) (p < 0.001). In the group with BAC, a higher proportion of patients were diabetics, hypertensives and had attained menopause, then in the subgroup without BAC.
Conclusion:
Patients with BAC had higher C-IMT, which in turn correlates with a higher risk of cardiovascular events. Hence, the presence of BAC can be used as a substitute marker for identifying patients with a higher risk of cardiovascular events and for ruling out co-morbidities such as DM and HTN.
Keywords
Breast arterial calcification
Carotid intima-media thickness
Hypertension
Diabetes
Menopause
Introduction
The importance of predicting adverse cardiovascular events and its value in preventing morbidity and mortality needs no further substantiation, a useful tool in this regard is the carotid intima-media thickness (C-IMT). The C-IMT reflects the degree of atherosclerosis in the wall of the carotid artery. It is a proven surrogate marker of coronary artery disease and is a predictor of risk of adverse cardiovascular events. The C-IMT can be easily and accurately measured using B-mode ultrasound. The ultrasonographic measurement of C-IMT is noninvasive, quick, reproducible, and inexpensive – all properties of an appropriate screening tool.[1,2]
C-IMT is an independent predictor of hypertension (HTN), diabetes mellitus (DM), cardiac health, and also associated with menopause.[3,4-7]
While all patients may not undergo neck ultrasound or carotid artery Doppler, many women, especially those above 40 years, do undergo mammograms. American College of Radiology recommends screening mammograms for all women above 40 years of age for carcinoma screening. BAC (breast arterial calcification) is often an incidental finding on mammograms.[8] BAC, identified as rail–road calcifications due to their classical parallel linear appearance on mammograms, signify calcific medial sclerosis of medium-sized arteries.[9] Since atherosclerotic changes occur throughout the vasculature, calcifications in the walls of the arteries that supply to the breast could potentially reflect the calcifications of other major vessels, and in turn, predict the risk of cardiovascular events.
Various studies showed the relationship between BAC with HTN,[10] DM,[11] coronary artery diseases,[12] carotid plaques,[13] dyslipidemia,[14] visceral obesity,[14] and chronic kidney disease.[15] However, the studies establishing the relationship between BAC and C-IMT have been rather limited.[3,16-17]
Therefore, to test the above hypothesis, we analyzed the relationship between BAC on mammography with C-IMT – a proven marker of cardiovascular risk. We also assessed the relationship in subsets including patients with comorbidities (HTN and DM) and menopausal status with BAC.
Materials and Methods
We conducted a hospital-based observational study from April 2021 to October 2021 in the Department of Radiology, Sri Ramachandra Institute of Higher Education and Research. Institutional ethics approval was obtained (CSP-MED/21/APR/68/62). Informed consent was obtained from all participants. Women above the age of 40 years who underwent screening and diagnostic mammograms at our institution were included in the study.
The minimum estimated sample size to achieve a power of 80% at a 5% level of significance was calculated as 126 participants with 63 in each group. As it was planned to study the results in different subgroups – DM, HTN, and menopausal status, we decided to include 540 participants, out of which 270 participants were with BAC and an equal number without BAC.[18]
Phase 1: Mammogram was done using a Fuji Amulet X-ray Mammography unit and standard mammographic views [cranio-caudal (CC) and mediolateral oblique (MLO) views] were obtained in all patients. Mammograms were interpreted independently by two trained radiologists who had an experience of 20 and 15 years. Breast arterial calcifications were identified as rail–road calcifications due to their classical parallel linear appearance on mammograms.
Co-morbidities and clinical history including DM, HTN, heart disease, menopausal history, and history of previous surgery were noted.
After obtaining informed consent, participants were enrolled in the study until the desired number of participants with and without BAC was achieved.
Phase 2: After the mammogram, the participants underwent ultrasound evaluation of the carotid arteries with Toshiba Apollo 500 unit with an 8-13 MHz linear transducer. The C-IMT was measured in bilateral common carotid arteries 1 cm proximal to the carotid bulb.
Ultrasound of bilateral carotid arteries for C-IMT was performed by two trained radiologists independently who had an experience of 10 and 19 years. Radiologists performing ultrasonography (USG) were unaware of the presence or absence of BAC on mammograms. The patient was positioned in the supine position and a pillow was placed below the shoulders to hyperextend the neck. The patient’s neck was turned to 45 degrees, on the contralateral side of the examination. The common carotid arteries were traced through their lengths on both sides up to the bulb. Intima-media thickness was measured at approximately 1 cm proximal to the bulb by placing the transducer along the longitudinal axis of the carotid arteries. The C-IMT was measured using a caliper in B-mode ultrasound. Two arterial layers are seen separately, intima seen as the echogenic layer, and media seen as the echo poor layer. Both were included in the measurement. Mean C-IMT of bilateral common carotid arteries was considered.
Statistical Analysis: The data was entered into Microsoft Excel and analyzed in R version 4.0.2.[19] Descriptive analysis was performed, and results were represented as percentages for categorical variables, as median and interquartile ranges for quantitative variables. The mean C-IMT values of bilateral common carotid arteries, of participants with and without BAC, were compared using the Mann–Whitney U test. For comparing the proportion of factors like DM, HT, and menopausal status, within patients with and without BAC, a Chi-square test was done. Binary logistic regression was done to identify the role of confounding DM, HT, and menopause with each other, and an adjusted odd ratio with 95% CI was computed. A p-value of less than 0.05 was considered to be statistically significant. Similar analyses were carried out within subsets of patients with and without DM, HTN, and age less than and more than 50 years to determine the association between BAC and C-IMT in these subsets.
Results
The study included a total of 540 participants aged between 40-80 years.
The median age in participants with BAC was 57 years (IQR = 10) and that in participants without BAC was 48 years (IQR = 11.75). Higher proportion of women with BAC had HTN and were post menopausal [Table 1].
| Sr. No. | Characteristic | BAC | p-value | |
|---|---|---|---|---|
|
Yes (n = 270) |
No (n = 270) |
|||
| 1 | Age 50 years and above | <0.001 | ||
| Yes | 223 (82.6%) | 127 (47.0%) | ||
| No | 47 (17.4%) | 143 (53.0%) | ||
| 2 | Post-menopausal | <0.001 | ||
| Yes | 228 (84.4%) | 136 (50.4%) | ||
| No | 42 (15.6%) | 134 (49.6%) | ||
| 3 | Diabetes | <0.001 | ||
| Yes | 160 (59.3%) | 48 (17.8%) | ||
| No | 110 (40.7%) | 222 (82.2%) | ||
| 4 | Hypertension | <0.001 | ||
| Yes | 122 (45.2%) | 42 (15.6%) | ||
| No | 148 (54.8%) | 228 (84.4%) | ||
BAC: Breast Arterial Calcification
The median C-IMT was higher in participants (as evident in sample cases in Figures 1 and 2) with BAC 0.85 mm, IQR = 0.20 than in the participants without BAC 0.6 mm, IQR = 0.15. The difference was statistically significant with p-value = <0.001
RCC: right cranio-caudal, RMLO: right medio-lateral-IMT, C-IMT: carotid intima media thickness, CCA: common carotid artery.
To study the relationship of each variable with BAC, logistic regression was performed with calcification as the dependent variable, and age, diabetes, and HTN as independent variables in the model, as each variable could confound the relationship with the other. Menopausal status was not included in the model due to its collinearity with age. The logistic regression model was significant with p-value <.001. The individual variables which were significant were for age (p<0.001) and diabetes (p<0.001) [Table 2].
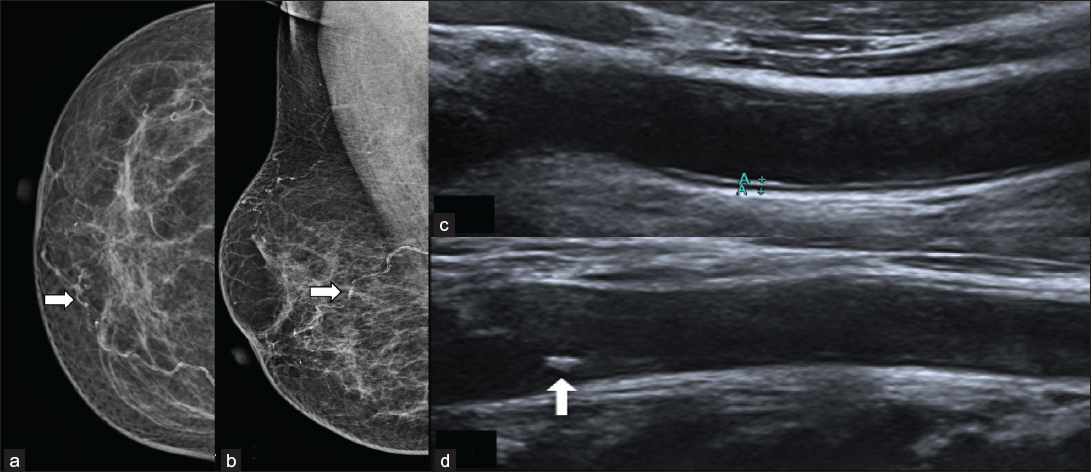
- A 69-year-old post-menopausal female with known diabetes mellitus, hypertension (HTN). On screening mammogram (a) RCC view and (b) RMLO view on mammogram shows rail road breast arterial calcification (white arrows). On ultrasound of neck (c) the C-IMT was 0.09 cm in right CCA and (d) the C-IMT was 0.01 cm with a plaque (white arrow) is seen in left CCA.

- A 47-year-old female with known diabetes mellitus, hypertension. Screening mammogram (a) LCC view and (b) LMLO view on mammogram shows rail–road breast arterial calcification (white arrows). On ultrasound of the neck (c), the C-IMT was 0.01 cm in the right CCA with a plaque (white arrow) and (d) the C-IMT was 0.08 cm in the left CCA.
- LCC: left cranio-caudal, LMLO: left medio-lateral-IMT: carotid intima media thickness, CCA: common carotid artery.
| Sr. No. | Characteristic |
Crude OR (95%CI) |
Adjusted ORa |
|---|---|---|---|
| 1 | Age 50 years and above | 5.3 (3.6–8.0) | 3.4 (2.2–5.2) |
| 2 | Attained menopause | 5.3 (3.6–8.0) | - |
| 3 | Diabetes | 6.7 (4.5–10.0) | 4.3 (2.8–6.8) |
| 4 | Hypertension | 4.5 (3.0–6.8) | 1.6 (0.97–2.6) |
OR: odds ratio, ORa: adjusted odds ratio for age, diabetes, and HTN.
As age and diabetes were important factors in the model, subgroup analysis of the relationship between C-IMT and calcification was carried out based on age categorization (age ≥50) and the presence of diabetes. It was observed that the median C-IMT is higher in those with BAC across all the subgroup analyses. All the results were found to be statistically significant at p<0.001.
Discussion
Our study showed that median C-IMT in patients with BAC (0.85 mm) was significantly higher than those without BAC (0.6 mm), p < 0.001. C-IMT of 0.7 mm was considered as the cutoff value.[20] A significantly higher proportion of women with BAC (98.5%) had C-IMT > 0.7 as compared to women without BAC (37.5%) (p < 0.001). This is in concordance with previous studies which showed significant differences in C-IMT in participants with and without BAC, with mean C-IMT of 0.86 ± 0.21 mm and 0.71± 0.12 mm in patients with and without BAC, respectively[20] (p < 0.001). Another study showed mean C-IMT (0.81 mm, SD ± 0.2) and (0.69 mm, SD = 0.2) in patients with and without BAC, respectively.[21]
An increase in C-IMT is a measure of carotid atherosclerosis due to the involvement of the intimal and medial layers of the artery.[22] Multiple studies have shown the correlation of C-IMT with atherosclerosis and cardiovascular events.[20,23-24] Hence, C-IMT is an established surrogate marker of cardiovascular diseases, which can be easily evaluated on ultrasound.
Most patients with atherosclerosis do not experience overt symptoms clinically, thus increasing the sudden mortality by >50% because of cardiac diseases.[25] We aimed to determine if the presence or absence of BAC correlated with C-IMT and with different variables like age, DM, HTN, and menopause.
The mean age of patients with BAC (57 years) was higher than patients without BAC (49 years). BAC was more common in participants with increased age >50 years, which is statistically highly significant (p < 0.001). This agrees with other studies that found a significant difference between the mean age of women with and without BAC.[16,26] About 84.4% of post-menopausal women in our study had BAC on mammograms. This was similar to other studies showing a significant correlation of BAC with menopause.[17,21]
The majority of women (n = 160, 60.6%) with BAC suffered from DM, among which six had type I DM and the rest had type II DM. A total of 48 (17.8%) women without BAC had DM, among them 12 had recently been diagnosed with mild DM and 2 were prediabetics. A significant association was found between BAC similar to the results shown by Kemmeren JM et al.[21] showing prevalence of BAC was 60% higher in diabetics compared to nondiabetics in a study of 12,239 patients within the age group of 50–68 years. In another study with 307 patients, diabetes was seen in 95 women with BAC and 64 without BAC, demonstrating no significant correlation (p = 0.75).[14]
A total of 122 women in our study with BAC were hypertensive showing a statistically significant correlation of HT with BAC (p-value<0.001). Similarly, Laurie Margolies et al.[27] demonstrated an association of BAC with HT with 90 out of 124 women with BAC having HTN (p<.001).
Conclusion
Breast arterial calcification is an incidental finding in mammograms, and it does not have many significant implications pertaining to the breast itself. However, it is understandably a reflection of arterial calcifications elsewhere in the body, including that in major vessels that supply vital end organs.
Our study shows that the presence of BAC has a statistically significant correlation with increased C-IMT, an established marker of cardiac mortality and morbidity. In addition, an independent correlation of BAC was seen with diabetes and menopause.
The clinical association of BAC with C-IMT instates the importance of active evaluation and reporting of BAC on mammograms in paving the way for further evaluation for these co-morbidities, thus allowing for early lifestyle modifications, pharmacotherapy, and interventions as needed to potentially prevent or reduce the incidence of future cardiovascular events.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Ethical approval
The author(s) declare that they have taken the ethical approval from IRB/IEC.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Ultrasonographically assessed carotid morphology and the risk of coronary heart disease. Arterioscler Thromb. 1991;11:1245-9.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment and relevance of carotid intima-media thickness (C-IMT) in primary and secondary cardiovascular prevention. Curr Pharm Des. 2015;21:1164-71.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Breast arterial calcification and risk of carotid atherosclerosis: focusing on the preferentially affected layer of the vessel wall. Eur J Radiol. 2011;79:250-6.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of carotid intima-media thickness in hypertensive patients and control group. J Cardiovasc Echography. 2016;26:48-51.
- [Google Scholar]
- A multifactorial approach in type 2 diabetes over 3 years decelerates progression of subclinical arterial disease in routine clinical practice. Angiology. 2021;72:923-33.
- [CrossRef] [PubMed] [Google Scholar]
- Difference in carotid intima-media thickness between pre and postmenopausal women. Menopause N Y N. 2019;26:39-44.
- [Google Scholar]
- Carotid intima-media thickness in patients with hyperuricemia: a systematic review and meta-analysis. Aging Clin Exp Res. 2021;33:2967-77.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Breast arterial calcifications as an indicator of systemic vascular disease. Acta Radiol Stockh Swed 1987. 2004;45:726-9.
- [Google Scholar]
- Monckeberg medial calcific sclerosis mimicking malignant calcification pattern at mammography. J Clin Pathol. 2005;58:447-8.
- [Google Scholar]
- Prevalence of breast arterial calcification in hypertensive patients. Clin Radiol. 2004;59:92-5.
- [CrossRef] [PubMed] [Google Scholar]
- Breast arterial calcification in association with diabetes mellitus: Too weak a correlation to have clinical utility. Radiology. 1985;155:577-9.
- [CrossRef] [PubMed] [Google Scholar]
- The association of breast arterial calcification and coronary heart disease. Obstet Gynecol. 2011;117:233-41.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluating the association between breast arterial calcification and carotid plaque formation. J Breast Health. 2015;11:180-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The association of breast arterial calcification and metabolic syndrome. Clin Sao Paulo Braz. 2014;69:841-6.
- [Google Scholar]
- Breast arterial calcification: A marker of medial vascular calcification in chronic kidney disease. Clin J Am Soc Nephrol CJASN. 2011;6:377-82.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Association of breast arterial calcification and carotid intima-media thickness. Heart Vessels. 2008;23:376-82.
- [CrossRef] [PubMed] [Google Scholar]
- Association of vascular calcification of breast with carotid intima media thickness. Pol J Radiol. 2019;84:e335-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- OpenEpi Menu. Available from: https://www.openepi.com/Menu/OE_Menu.htm [Last accessed on 2021 Dec 25].
- R: The R Project for Statistical Computing. Available from: https://www.r-project.org/ [Last accessed on 2021 Dec 25].
- Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA) Arch Intern Med. 2008;168:1333-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Breast arterial calcifications: association with diabetes mellitus and cardiovascular mortality. Work in progress. Radiology. 1996;201:75-8.
- [Google Scholar]
- Ultrasound markers of carotid atherosclerosis and cognition: The Northern Manhattan study. Stroke. 2017;48:1855-61.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The role of carotid intimal thickness testing and risk prediction in the development of coronary atherosclerosis. Curr Atheroscler Rep. 2013;15:306.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Carotid-wall intima–media thickness and cardiovascular events. N Engl J Med. 2011;365:213-21.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Executive summary: heart disease and stroke statistics–2014 update: A report from the American Heart Association. Circulation. 2014;129:399-410.
- [CrossRef] [PubMed] [Google Scholar]
- The timing of the age at which natural menopause occurs. Obstet Gynecol Clin North Am. 2011;38:425-40.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Digital mammography and screening for coronary artery disease. JACC Cardiovasc Imaging. 2016;9:350-60.
- [CrossRef] [PubMed] [Google Scholar]